The lower cervical spines, C
3-7 segments, are the predilection sites of cervical trauma, and the fracture and dislocation on these sites is the compound violent injury with high-energy, which is the main reason for spinal cord injury.
Timing for surgery of lower cervical spine fracture and dislocation
Spinal cord injury is divided into two pathological processes of primary and secondary injury. The primary injury is determined with the nature of injury that cannot be changed; while the secondary injury is the series reaction of tissue cells to trauma, such as hemorrhage, edema and microcirculation, including neurotransmitter endogenous opioid increasing, cell apoptosis accelerating and nitric oxide and excitatory amino acid increasing, and the secondary injury occurred based on the primary injury can further aggravate spinal cord injury
[10] . The main purpose of the treatment of spinal cord injury is to recover the function of conduction system in the spinal cord white matter as early and fast as possible, and prevent the secondary injury at the same time. A present, most of the scholars advocate the early surgical treatment in order to shorten time of spinal cord compression, improve microcirculation, clean the accumulation of oxygen free radicals generated after injury and reduce the cytotoxic effect of peroxide and calcium conduction, and other secondary injury. Domestic and foreign scholars’ studies showed that early surgical decompression was negative correlated with the recovery of spinal cord neurological function and the treatment time
[11-12] , therefore, most scholars advocate to have surgery in 8 hours, and no later than 24 hours, otherwise, delay for 1 week as the surgery in 3 days has little value
[13-17] , but the early surgery may increase the risk of iatrogenic damage of spinal cord edema.
Among the 12 patients in this study, only one patient had surgery in 24 hours after injury, four patients had surgery in 24-72 hours after injury, and seven patients had surgery in 72 hours to 8 days after injury. The decompression surgery performed in 12 patients in 24 hours after injury could not achieved, the reasons were: high fever, patients with cervical spine fracture and dislocation had continued fever in 3-12 hours after injury, the body temperature often > 39 ℃, which easy to lead to serious complications such as dehydration and cerebral edema; sinus bradycardia, in 1 week after spinal cord injury, the spinal sympathetic descending pathways were interrupted and transitory atrophy occurred in the sympathetic preganglionic neurons without influence on vagus nerves, all these complications may result in tone imbalance between sympathetic and parasympathetic, baroreflex vagal bradycardia occurred, and cardiac arrest may occurred in serious patients; orthostatic hypotension, sympathetic dysfunction after apinal cod injury may also cause peripheral vasodilation, if combined with diet restricted and dehydration therapy, the blood volume of the patients was relative or absolute insufficient, which may lead to severe orthostatic hypotension with life-threatening. So, in clinic, the timing for surgical treatment should be selected according to the conditions of the patients, generally the surgery was performed at 7 days after injury, and the methylprednisolone could be used before vertebral open decompression during surgery in order to reduce the incidence of secondary injury.
Surgical approach of lower cervical spine fracture and dislocation
The patients may has cervical derangement, instability and cervical disc rupture and highlight due to the cervical structural damage at the moment of spinal cord injury, and the vertebral fracture and dislocation often occurs on the vertebral back edge and the anteroposterior spinal cord, thus leading to cervical spinal cord injury and compression. Therefore, the treatment of cervical fracture and dislocation has to completely remove the spinal cord compression, restore the cervical lordosis, restore the intervertebral height and canal volume, reconstruct the cervical stability and maintain the steady state, and thus achieve osseous fusion. At present, the anterior cervical decompression surgery has been widely used, and the patients in this group are suitable to select the anterior cervical surgery. The clinical treatment results showed that anterior cervical surgery has become the ideal method for the treatment of cervical fracture.
The 12 patients in this group have cervical spinal cord injury on the compression segment caused by cervical fracture, cervical disc herniation and anterior compress the spinal cord, or caused by the oppression of hematoma and bone fragments exist in front of the cervical spinal cord. In order to avoid the deterioration of spinal cord neurological function or even the permanent loss of spinal cord neurological function caused by injured intervertebral disc, bone fragments and hematoma going into the spinal canal during reduction, we will directly resect the pressure through anterior approach, such as fracture fragments or intervertebral disc tissue, that inrush into the spinal canal under direct vision, in order to cure cervical spinal cord compression; meanwhile, the ADD plus-winged adjustable device was used to regulatory recover the intervertebral height, physiological curvature and spinal canal capacity, thus reconstruct the stability of spine. We also found that the anterior approach is simple to operate with less postural changes, and can reduce the further spinal cord injury; the anterior approach has the advantages of small surgical trauma, less bleeding and relative short operative time, and the operation can accelerate the healing time, which is easy for decompression and anatomic reduction; the depressor that cause pressure on the rear edge of vertebral body can be depressed directly and thoroughly; anterior approach operation can restore the normal cervical intervertebral height and physiological curvature with less fusion segment, low incidence of neck pain, and has less effect on the cervical spine activity.
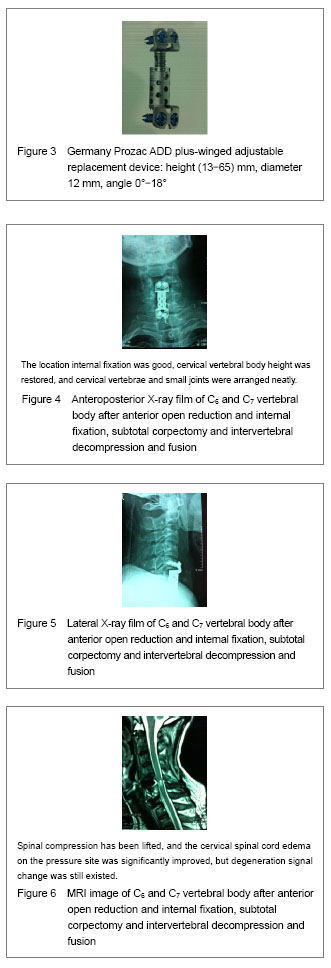
Characteristics of anterior approach ADD plus-winged adjustable replacement device
The ADD plus-winged adjustable replacement device is made of pure titanium with good biocompatibility and low allergic reactions, and will not influence the postoperative MRI examination. Winged distraction vertebral body replacement device is suitable for cervical vertebrae and thoracic vertebrae, and the different tilt angles of the upper and lower wing of cervical vertebrae prosthesis can meet the physiological structure of cervical vertebrae to the maximum extent. The support surface of the wings is the flat design, which can be fixed on the vertebral body with the single or double cortex screws, in order to decrease the risk of collapse and can keep a safe distance between screw and end plate. The distraction height can be adjusted freely in order to restore the intervertebral foramen height and better repair the vertebral defect. It is simple and safe for implantation, and it can support and fix the spine in the same time, the window design makes the fusion block and adjacent vertebral bodies contact directly. The ADD plus-winged adjustable replacement device is suitable for C
3-T
3 multi-segment fusion, and suitable for repair of vertebral defect caused by tumor or fracture, as well as the instability caused by vertebral total resection and vertebral subtotal resection.
Treatment and prevention of the intraoperative and postoperative complications of lower cervical spine fracture and dislocation surgery
High fever: for the patients with the temperature of 39 ℃-40 ℃, continued ice or alcohol sponge bath physical cooling should be performed, and then received intramuscular injection of 2 mL bupleurum; the patients with the high fever of 40 ℃ subside should be treated with intramuscular injection of analgin; the patients with the temperature of 41 ℃ or above can be treated with lytic cocktail therapy; the dehydration, cerebral edema and other serious complications should be monitored. Patients with sinus bradycardia can use ß-adrenergic receptor agonists (such as salbutamol) to activate cardiac sympathetic nerve activity. Orthostatic hypotension: moderate blood transfusion or rehydration can be performed to supplement the blood volume of patients with relative or absolute blood volume shortage, and to avoid and reduce the incidence of orthostatic hypotension. Hyponatremia: acute cervical spinal cord injury, especially high cervical cord injury caused hyponatremia is usually intractable that difficult to correct. The more serious the cervical spinal cord injury is, the higher the incidence of hyponatremia, and the more severe the degree; the hyponatremia often occurs at 1 week after cervical spinal cord injury and lasted for 2-4 weeks, but there was one patient had hyponatremia at 1 week after operation and in light coma situation, which is considered to be the syndrome of inappropriate antidiuretic hormone secretion, so the patients should strictly limit the intake of water during the treatment, and pay attention to the sodium supplement; moderate sodium supplement combined with hydrogen fluoride cortisone drugs and colloid replacement therapy has significant effect. Pulmonary embolism: early diagnosis is difficult, and it is the dangerous disease with high mortality rate. Approximately 85% of the emboli caused by the deep venous thrombosis, and the best treatment method was prevention, including promotion of local blood circulation with lower extremity venous pump, and the prevention of blood viscosity increasing with the anticoagulant drugs of rivaroxaban and aspirin; the elderly patients and the patients with cardiovascular and cerebrovascular diseases and dyslipidemia received vascular B-ultrasound examination before operation, and positive patients will placed with inferior vena cava network. Cervical hyperextension caused the patient’s injury aggravation should be prevent during preoperative systemic anesthesia intubation; during intraoperative incision and tissue separation, anatomical level should be cleared in order to avoid damage to the blood vessels and nerve; during ligation and hemostasis, the ends should be ligated firstly, and then cutting the middle to prevent air embolism; using the retractor without excessive force, in order to avoid recurrent laryngeal nerve and esophagus stretch injury; gentle operation to avoid spinal cord injury and dural sac, and the decompression range should not be too large, so as not to damage the vertebral artery; the location of screws should be accurate to avoid screwing into the intervertebral space and lead to loose and quit; postoperative incision drainage should be keep unobstructed, in order to prevent deep neck hematoma formed oppression and thus resulting in respiratory depression.
Cervical spine fracture and dislocation with spinal cord injury treated with ADD plus-winged adjustable replacement system
At present, anterior cervical decompression combined with bone graft surgery has become the effective treatment method for lower cervical spine trauma, and with the clinical development and application of this surgical method, many clinicians pay more and more attention on the long-term follow-up effect, as well as the observation of cervical spine degeneration of the fusion segments and adjacent segments. Baba et al
[18] analyzed the images of the 106 patients treated with anterior cervical decompression combined with bone graft internal fixation at 8.5 years after operation and found that about 1/10 patients had increased range of motion on the fusion and adjacent segments, and lead to the increased stress on the fusion and adjacent segments, thus resulted in degeneration. Gore et al
[19] performed 21-year follow-up on 146 patients treated with anterior cervical decompression combined with bone graft internal fixation and found that 33% patients had degeneration of the fusion and adjacent segments and then exhibited symptoms of spinal cord injury. Goffin et al
[20] studied on 25 cervical spine fracture and dislocation patients who treated with anterior cervical plate fixation, and all the patients had 5-9 years follow-up, finding that 15 patients had forward degeneration on the adjacent segment in the fusion range that may be caused by too large plate model or improper location, and that may be related with the time, and emphasized the cervical spine healthcare at 24 months after strengthening surgery. The domestic scholar Zeng et al
[21] has proposed that pseudarthrosis formation is the common long-term complications after anterior cervical surgery, the incidence of pseudarthrosis formation has relationship with the number of fusion segment to some extent, and the pseudarthrosis formation may affect the postoperative long-term recovery of neurological function, but has no obvisou relationship with the postoperative neck symptoms. In conclusion, the treatment of lower cervical spine fracture and dislocation associated with spinal cord injury with anterior cervical fixation and fusion by ADD-plus winged adjustable system can overcome the excessive integration resulted with adjacent cervical segment degeneration bone bridge formation caused by too long length of the previous anterior plate fixation. Of course, even short-segment fixation and fusion, from the short-term clinical observation, there still exists fixed segment degeneration, the more the fusion segment is, the higher the incidence of degeneration, and the pseudarthrosis formation is more easy. Therefore, during the application of ADD-plus winged adjustable system, we should try to avoid long segment fusion and fixation; during the operation, we should correct the fracture dislocation and give moderate distraction height on the basis of maintaining the full restoration of canal volume with cervical spinal cord decompression, the excessive distraction and height and distance variation between the cervical vertebra should be avoided, in order to play the role of anterior fixation fusion and can decrease the incidence of cervical segment joint formation or cervical degeneration.
The author only screened 12 cases for the research, which is insufficient in sample size for the clinical observation, so the further clinical practice and the accumulation and summary of information is required; on the other hand, all the 12 cases in this group had anterior short segment fusion and fixation, and there is no three segments or above fusion, so that the 16.7% incidence of pseudarthrosis formation do not have a very accurate representation and persuasive. But it can still propose that anterior cervical fixation and fusion combined with bone graft cannot avoid pseudarthrosis formation completely, and it can confirm the comparative finding of the previous studies (the less the cervical segment fusion is, the lower the incidence ofpseudarthrosis formation). Observation from the repairing of cervical spinal cord injury, three cases with complete cervical spinal cord injury of the 12 patients have no obvious signs of cervical spinal cord recovery during follow-up period, the other nine cases with incomplete cervical spinal cord injury have relative large repairing of cervical spinal cord injury; the sensation and motion Frankle grading of two incomplete cervical spinal cord injury patients were recovered from C and D grade to E grade, three cased recovered to the D grade. Observation from the bone fusion, all the 12 patients treated with ADD-plus winged adjustable system achieved bone fusion in 11 months after operation, which was slightly longer than the 6-8 months reported in the previous study, that may be related with various factors, such as severity of fracture and dislocation, physique and age of the patients, nutritional status, bone graft and postoperative neck healthcare.
In summary, anterior cervical decompression and fusion can fully discharge the cervical spinal cord mechanical pressure, which is the main condition for promoting recovery of neurological function of spinal cord. The application combined with flexible and convenient ADD-plus winged adjustable system can bring safe, secure and reliable clinical protection to the patients with lower cervical spine fracture and dislocation combined with spinal cord injury.